5 Questions Hospitals Ask Before Choosing EMR Software
The selection of an Electronic Medical Record (EMR) system is not merely a procurement exercise; it is the most significant operational commitment a hospital leadership team will ever undertake.
In the corridors of health system administration, we often refer to this as the “billion-dollar handshake.” This moniker reflects the reality that once a contract is signed, the hospital is inextricably bound to a technology partner for the next decade or more.
This decision defines the central nervous system of your entire healthcare ecosystem, influencing every clinical touchpoint and administrative workflow.
However, the sheer gravity of this choice often leads to a paralyzing phenomenon known as “choice paralysis.”
Faced with an overwhelming array of vendors, modular add-ons, and conflicting stakeholder demands, decision-makers often retreat into safe, brand-name choices that may not fit their specific needs.
This hesitation is understandable because the stakes are uniquely high in medicine. A poorly chosen EMR is not just a frustrating software experience; it is a systemic inhibitor that creates friction between the clinician and the patient.
When the technology fails to align with the reality of the ward, the consequences are immediate and measurable. We see a spike in clinician burnout, as doctors and nurses are forced to sacrifice “eyes-on-patient” time for “eyes-on-screen” documentation.
This digital friction erodes morale and can lead to the departure of your most talented clinical staff. Furthermore, an inefficient system introduces cognitive fatigue, which is a primary driver of medical errors and reduced patient through put.
Choosing the right EMR requires moving past the polished marketing demonstrations and focusing on the underlying architecture of the partnership.
It is about asking the fundamental, high-stakes questions that determine whether a system will be a silent partner in healing or a loud obstacle to care.
This document provides a strategic framework based on the five critical questions every hospital must ask. By focusing on these pillars, leadership can shift from a state of technological anxiety to a position of operational clarity.
Question 1: How Does the System Align with Our Specific Clinical Workflows?
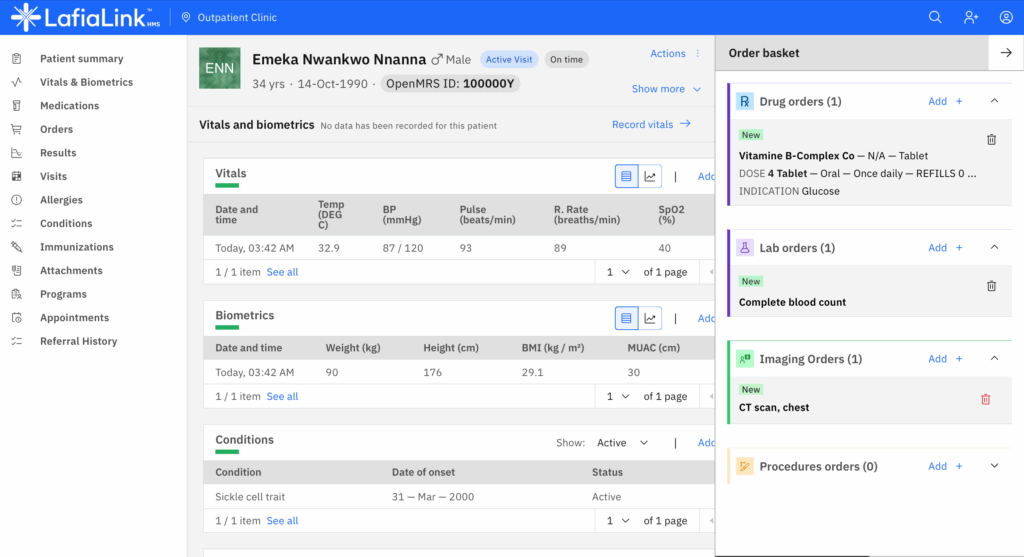
The most vital concern in any EMR selection is the degree of alignment between the software and the actual movements of clinical staff. An EMR should never be a passive digital filing cabinet; it must be an active participant in the care process that understands the tempo of the floor.
If a system requires a Level 1 Trauma surgeon to navigate the same UI logic as a primary care pediatrician, the architecture has already failed.
Usability is not a “nice-to-have” feature; it is a core clinical safety requirement that determines the success of the entire digital transformation.
Hospitals must evaluate how the system handles the unique nuances of diverse departments, from the high-velocity environment of the Emergency Department to the longitudinal complexity of Oncology.
When a system is overly rigid, clinicians are forced to develop “workarounds,” which are the unofficial, manual processes used to bypass software limitations.
These workarounds are dangerous because they create data silos and fragmentation. If critical patient information exists only on a sticky note because the EMR was too slow to update, the integrity of the patient record is compromised.
“The true measure of a clinical system is its ability to move at the speed of human thought, ensuring the technology serves the healer rather than the healer serving the machine.”
The long-term impact of ignoring workflow alignment is a steady increase in clinician disengagement. “Death by a thousand clicks” is a literal description of the cognitive load placed on staff when a simple medication order requires multiple screen transitions.
Over a standard twelve-hour shift, this cumulative friction leads to profound exhaustion.
By prioritizing clinical alignment during the selection phase, hospital leaders protect their most valuable asset: the focus and well-being of their medical professionals.
This alignment also extends to the “frictionless” entry of data, where the system anticipates the next step in a clinical pathway. A well-designed EMR uses intuitive UI/UX principles to reduce the mental energy required to document care.
This allows the physician to remain present with the patient, fostering the human connection that is essential for effective diagnosis and treatment. When the software fits the workflow, the technology becomes invisible, allowing the mission of care to take center stage once again.
Question 2: Does This System Enable True Interoperability Across the Care Continuum?
In our modern, interconnected healthcare landscape, a hospital can no longer afford to operate as a closed data island. Patients move fluidly between various care settings, including retail clinics, specialist offices, and home health environments.
The second critical question focuses on “data liquidity” the ability of information to flow securely and seamlessly across different platforms.
Interoperability is no longer just about sending a digital fax; it is about the real-time exchange of actionable intelligence using modern standards like FHIR (Fast Healthcare Interoperability Resources) APIs.
For a nurse on a busy medical-surgical floor, interoperability is a lifeline that provides the full picture of a patient’s journey.
Consider an unconscious patient arriving in the ER with no family present; a truly interoperable system can instantly query the Trusted Exchange Framework and Common Agreement (TEFCA) network to pull a comprehensive history.
This includes recent lab results, current prescriptions, and documented allergies from external systems.
Without this capability, clinical teams are forced to make high-stakes decisions based on incomplete or outdated information.
“Data that remains trapped within a single system is a liability; data that moves with the patient across the continuum of care is a clinical asset.”
The absence of robust interoperability leads to the creation of “data silos,” where valuable insights are locked behind proprietary vendor walls.
This results in significant operational waste, such as redundant diagnostic imaging and laboratory testing, because clinicians cannot see results from other facilities.
These redundancies drive up the total cost of care and delay the initiation of treatment. Selecting a system built on open standards ensures that your hospital remains a vital, connected node in the broader healthcare ecosystem.
Furthermore, interoperability is the foundation for future innovation in population health management. If your EMR cannot easily ingest data from wearable devices or remote monitoring tools, you will be unable to compete in a value-based care environment.
A system that prioritizes the “care continuum” allows your hospital to manage the patient’s health long after they have been discharged.
This proactive approach is essential for reducing readmission rates and improving the overall health of the community you serve.
Question 3: What is the Total Cost of Ownership Over the Next Decade?
The financial reality of EMR selection extends far beyond the initial licensing fee or the “sticker price” presented during the sales cycle.
This question requires a rigorous analysis of the Total Cost of Ownership (TCO), accounting for the shift from traditional CapEx (Capital Expenditure) to modern OpEx (Operating Expenditure) models.
As the industry moves toward SaaS (Software as a Service) platforms, hospitals must understand the long-term cost implications of subscription-based pricing and cloud infrastructure.
A failure to account for these variables leads to “vendor lock-in,” where the cost of exiting a system becomes prohibitively expensive.
To avoid future technical debt, administrators must look at the specific cost drivers that accrue over the software’s lifecycle.
These are not just IT costs; they are operational costs that impact the entire hospital budget. Below are critical data points and industry benchmarks for TCO evaluation:
Annual Maintenance and Support: Typically ranges from 18% to 22% of the initial licensing cost for on-premise solutions.
Ongoing Staff Training: Hospitals should budget 10% to 15% of the total implementation cost for recurring education as new features are released.
Initial Productivity Dip: Expect a 20% to 30% reduction in clinical throughput during the first 90 days of “go-live.”
Hardware Refresh Cycles: For non-cloud systems, hardware must be upgraded every 3 to 5 years to maintain peak performance.
By analyzing these metrics, leadership can prevent the EMR from becoming a financial “black hole” that drains resources away from clinical facility improvements.
A well-vetted financial roadmap allows the hospital to maintain a sustainable margin while still investing in digital innovation. It ensures that the IT department is seen as a strategic partner in growth rather than a constant source of unbudgeted expense requests.
A strategist must also consider the cost of “technical debt”, the long-term expense of maintaining legacy integrations and outdated database structures.
If an EMR is built on an old codebase, the cost of adding new features or integrating AI tools will be significantly higher than with a modern, modular system. Selecting a vendor with a transparent roadmap and a modern architecture is a defensive financial move.
It protects the hospital against the massive “hidden costs” of trying to make old technology perform in a modern world.
Question 4: How Will This System Improve Measurable Patient Outcomes?
Ultimately, the primary justification for any massive technology investment in a hospital must be the improvement of patient health. The fourth question focuses on the relationship between the EMR’s architecture and the quality of clinical outcomes.
An effective system should do more than record the past; it should help shape a safer future through advanced Clinical Decision Support (CDS). This includes real-time alerts for sepsis, automated checks for drug-drug interactions, and standardized pathways based on the latest evidence-based medicine.
When an EMR is designed with an outcome-driven mindset, it serves as a digital safety net for the entire clinical team. For example, if a physician orders a medication that conflicts with a patient’s genetic profile or recent lab results, the system should trigger a “hard-stop” alert.
This proactive intervention prevents adverse drug events before they can reach the patient’s bedside. These systems can also use predictive analytics to identify deteriorating patients hours before their vitals show a traditional decline, allowing for early intervention.
“The gravity of EMR selection lies in its power to either obscure clinical insights or illuminate the path to better patient health through data-driven precision.”
Efficiency is an inextricable component of the outcome equation. When documentation burden is reduced through smart templates and voice-to-text integration, nurses spend more time at the bedside.
Increased “eyes-on-patient” time is directly correlated with higher patient satisfaction scores and a reduction in hospital-acquired infections. A system that prioritizes outcome-driven design is a statement of the hospital’s values, proving that technology is being used to fulfill the core mission of healing.
Furthermore, an outcome-focused EMR allows for the granular tracking of clinical performance across the entire institution. Leadership can identify which protocols are yielding the best results and scale those “best practices” across the system.
This creates a culture of continuous improvement, where data is used to empower clinicians rather than just monitor them. By asking how the system improves outcomes, you are ensuring that your digital transformation is an investment in human life, not just digital record-keeping.
Question 5: Is This Technology Scalable and Future-Proof?
The final question addresses the long-term vision and resilience of the hospital’s digital infrastructure. Technology in healthcare is evolving at an exponential rate, and a system that is “state-of-the-art” today can become a legacy burden in less than five years.
Scalability is the “impactful takeaway” that many hospitals overlook because they are understandably focused on solving the immediate pressures of today.
However, a system that cannot grow with your institution will eventually lead to a painful and expensive replacement process.
Future-proofing requires a deep dive into the vendor’s architectural philosophy.
Does the system use a monolithic design, or is it built on a modular, microservices-based architecture? A modular system allows you to swap out or upgrade specific components, such as a telehealth module or an AI diagnostic tool, without overhauling the entire EMR.
This flexibility is essential for a hospital that plans to acquire new clinics, expand bed capacity, or move toward advanced predictive analytics.
“A future-proof system is not defined by the features it has today, but by its ability to integrate the innovations of tomorrow without breaking the core workflow.”
This question ties the entire selection strategy together by focusing on the vendor’s commitment to innovation and stability. You must investigate whether the vendor is investing heavily in R&D or simply maintaining a legacy product for its existing customer base.
A forward-looking partner will have clear roadmaps for integrating ambient clinical intelligence, remote patient monitoring, and machine learning. These technologies are no longer science fiction; they are the tools that will define the next generation of high-performing hospitals.
Choosing a scalable system ensures that the hospital can pivot quickly in response to changes in the regulatory or clinical landscape. Whether it is a new government reporting requirement or a sudden shift in care delivery models, a flexible EMR is your greatest strategic asset.
By asking about scalability and future-proofing, you transition from a “buyer” of software to a “partner” in a long-term digital evolution. This final check ensures that the billion-dollar handshake you make today remains a firm and beneficial grip for decades to come.
QUESTION 6: Does It Meet Compliance and Security Requirements?
Critical Importance
Healthcare organizations operate under stringent regulatory requirements. Data breaches cost organizations over $5 million on average in:
System downtime
Regulatory fines
Legal costs
Reputation damage
Patient notification
Consequences include:
Criminal penalties
Loss of Medicare/Medicaid participation
Professional liability
Loss of patient trust
Major Regulatory Frameworks
HIPAA (Health Insurance Portability and Accountability Act)
HIPAA Rules and Requirements
| Rule | Purpose | Key Requirements |
|---|---|---|
| Privacy Rule | Protects patient information | Use/disclosure limitations; patient access rights; minimum necessary; authorization |
| Security Rule | Protects electronic health information | Administrative, physical, and technical safeguards; risk analysis |
| Breach Notification | Requires breach reporting | Individual, HHS, and media notification; documentation |
HIPAA Security Rule – EMR Requirements:
Administrative Safeguards:
- Security management with risk analysis
- Assigned security responsibility
- Workforce security and training
- Information access management
- Incident procedures
- Contingency planning
- Business Associate Agreements
Physical Safeguards:
- Facility access controls
- Workstation security
- Device and media controls
- Secure disposal procedures
Technical Safeguards:
- Access control (unique user IDs, automatic logoff, encryption)
- Audit controls
- Integrity controls
- Authentication
- Transmission security
ONC Certification:
- Validates standards compliance
- Required for incentive programs
- Verified on Certified Health IT Products List
21st Century Cures Act:
- Prohibits information blocking
- Patient access requirements
- API requirements for third-party apps
- Data portability mandates
Security Requirements
Encryption Requirements
| Type | Standard | Application |
|---|---|---|
| Data at Rest | AES-256 minimum | Database, file storage, backups |
| Data in Transit | TLS 1.2+ | Network communications, APIs |
| Backup | AES-256 | All backup media |
| S/MIME or PGP | Patient information | |
| Mobile Devices | AES-256 | Tablets, smartphones, laptops |
Access Controls:
Authentication Strength
| Method | Security Level | Use Case |
|---|---|---|
| Username/Password | Basic | Acceptable with strong requirements |
| Multi-Factor (MFA) | Strong | Recommended for all, required for remote |
| Biometric | Very Strong | High-security areas |
| Smart Cards | Strong | Providers; administrative access |
| Single Sign-On | Varies | Convenience across systems |
Authorization:
- Role-Based Access Control (RBAC)
- Principle of least privilege
- Regular access reviews
- Granular permissions
- VIP patient protections
Audit Trails:
Events Requiring Logging
| Event Category | Specific Events | Retention |
|---|---|---|
| Data Access | View, search, print, export | Minimum 6 years |
| Data Modification | Create, update, delete, merge | Minimum 6 years |
| Authentication | Logins, failures, password changes | Minimum 6 years |
| System Administration | Configuration, user management | Minimum 6 years |
| Security Events | Violations, alerts, potential breaches | Minimum 6 years |
Audit logs must be:
- Tamper-proof
- Searchable and filterable
- Exportable
- Include timestamp, user ID, action, patient ID
- Support real-time monitoring
Network Security:
Network Security Layers
| Layer | Technologies | Purpose |
|---|---|---|
| Perimeter | Firewalls, IDS/IPS | Prevent unauthorized access |
| Segmentation | VLANs, subnets | Limit lateral movement |
| Encryption | VPN, TLS, IPSec | Protect data in transit |
| Access Control | NAC, MAC filtering | Authorized devices only |
| Monitoring | SIEM, NetFlow | Detect threats |
| DDoS Protection | Rate limiting, scrubbing | Maintain availability |
Backup and Disaster Recovery:
Backup Best Practices
| Requirement | Specification | Rationale |
|---|---|---|
| Frequency | Daily incremental; weekly full | Minimize data loss |
| Encryption | AES-256 | Protect backup media |
| Offsite Storage | Geographically distant | Protect against disasters |
| Testing | Monthly restore tests | Verify recoverability |
| Retention | Minimum 6 years | Regulatory compliance |
| RPO | <24 hours (preferably <1 hour) | Acceptable data loss |
| RTO | <4 hours for critical systems | Acceptable downtime |
What Hospitals Should Ask Vendors
Compliance Questions:
“Is your system ONC-certified? For which edition and modules?”
“How do you ensure HIPAA compliance? Can you provide documentation?”
“Do you provide a Business Associate Agreement?”
“How do you handle compliance with changing regulations?”
“What certifications do you hold?” (HITRUST, SOC 2, ISO 27001)
“How do you support state-specific requirements?”
“How do you comply with 21st Century Cures Act?”
Security Questions:
“What encryption standards do you use?”
“How is user access controlled and audited?”
“What is your security incident response plan?”
“Where is data stored and how is it protected?”
“What are your backup and disaster recovery procedures?”
“How do you manage security updates and patches?”
“What security testing do you perform?”
“Have you experienced any breaches? How were they handled?”
“What security training do you provide our staff?”
Third-Party Certifications
Key Security Certifications
| Certification | Scope | Value |
|---|---|---|
| HITRUST CSF | Comprehensive security framework | Healthcare-specific; rigorous |
| SOC 2 Type II | Security, availability, confidentiality | Third-party validated; detailed report |
| ISO 27001 | Information security management | International standard; systematic |
| FedRAMP | Federal cloud security | Required for federal; rigorous |
| NIST 800-53 | Federal security controls | Rigorous framework |
Shared Responsibility Model
Typical Shared Responsibilities
| Security Area | Vendor | Customer |
|---|---|---|
| Infrastructure | Physical security; network security | Endpoint security |
| Application | Software vulnerabilities; updates | User account management |
| Data | Encryption; backup; DR | Data classification; authorized use |
| Access | Authentication infrastructure; MFA; logging | User provisioning; access reviews |
| Compliance | HIPAA infrastructure compliance | HIPAA privacy compliance; policies |
| Monitoring | Infrastructure monitoring; threat detection | Audit log review; reporting |
| Incident Response | Vendor-side investigation; notification | Customer-side investigation; patient notification |
Data Ownership and Portability
Essential Questions:
“Who owns the data?”
Acceptable: Patient/hospital owns; vendor is custodian only
Unacceptable: Vendor owns or shares ownership
“What happens to our data if we terminate?”
Must include: Standard format export; reasonable timeframe; data deletion verification
“Can we export data anytime in standard formats?”
Required by 21st Century Cures Act
Should include FHIR, HL7, CSV options
“What standard formats are available?”
Prefer FHIR, HL7, structured formats
Avoid proprietary formats only
HIPAA Penalties
HIPAA Civil Monetary Penalties
| Tier | Violation Level | Minimum | Maximum Per Violation | Annual Maximum |
|---|---|---|---|---|
| 1 | Unknowing | $100 | $50,000 | $1.5 million |
| 2 | Reasonable cause | $1,000 | $50,000 | $1.5 million |
| 3 | Willful neglect, corrected | $10,000 | $50,000 | $1.5 million |
| 4 | Willful neglect, not corrected | $50,000 | $50,000 | $1.5 million |
Criminal Penalties:
Unknowing: Up to 1 year imprisonment
False pretenses: Up to 5 years
Malicious harm/commercial gain: Up to 10 years
Red Flags
Compliance:
No or expired ONC certification
Unwilling to provide documentation
Won’t sign BAA or BAA with limitations
Vague about regulatory compliance
History of violations
Security:
Weak or no encryption
No MFA support
Limited audit trails
Poor vulnerability management
Won’t share security audits
Security features cost extra
History of undisclosed breaches
Liability limitations in contract
Data Control:
Vendor claims data ownership
Data export restrictions
Proprietary formats only
Expensive portability fees
Unclear deletion procedures
Synthesis: Moving Beyond the Checklist
These five questions should not be treated as separate, disconnected items on a procurement checklist. Instead, they form a cohesive framework for a fundamental shift in how hospital leadership views its digital infrastructure.
In the past, technology was often viewed as a tool, much like a heart monitor or an infusion pump, to be bought, used, and eventually replaced. Today, we must recognize that the EMR is a living partnership that evolves alongside the clinical practice.
When a hospital asks these questions, it triggers a dialogue between the IT department, the finance office, and the clinical leadership. This multidisciplinary collaboration is the true secret to a successful implementation.
It forces the institution to move away from “feature-chasing” and toward “value-seeking.” By viewing these questions as a unified framework, you ensure that every stakeholder is aligned on the same goal: providing the best possible care through the best possible technology.
A Final Thought for the Digital Ward
The journey to selecting a new EMR is demanding and fraught with high-stakes decisions, but it is also a unique opportunity to redefine your hospital’s future.
By focusing on workflow alignment, interoperability, financial sustainability, patient outcomes, and scalability, you can cut through the marketing noise. You can find a system that doesn’t just store records, but actively assists in the noble work of healing the sick.
As we look toward a future where predictive AI and genomic data become standard parts of the care process, the decisions made in the boardroom today will echo through the hallways for years.
The ultimate goal is to create a digital ward where the technology is so well-integrated that it becomes invisible. We want our clinicians to forget about the software and focus entirely on the person in the bed.
If your hospital were to go fully paperless tomorrow, would your current technology empower your doctors to save more lives, or would it simply give them more paperwork in a digital form?