What is an EMR System? A Complete Guide to Electronic Medical Records
Electronic Medical Records (EMR) systems have revolutionized how healthcare providers manage patient information.
But what exactly is an EMR system, and why has it become essential in modern medical practice?
Understanding EMR Systems
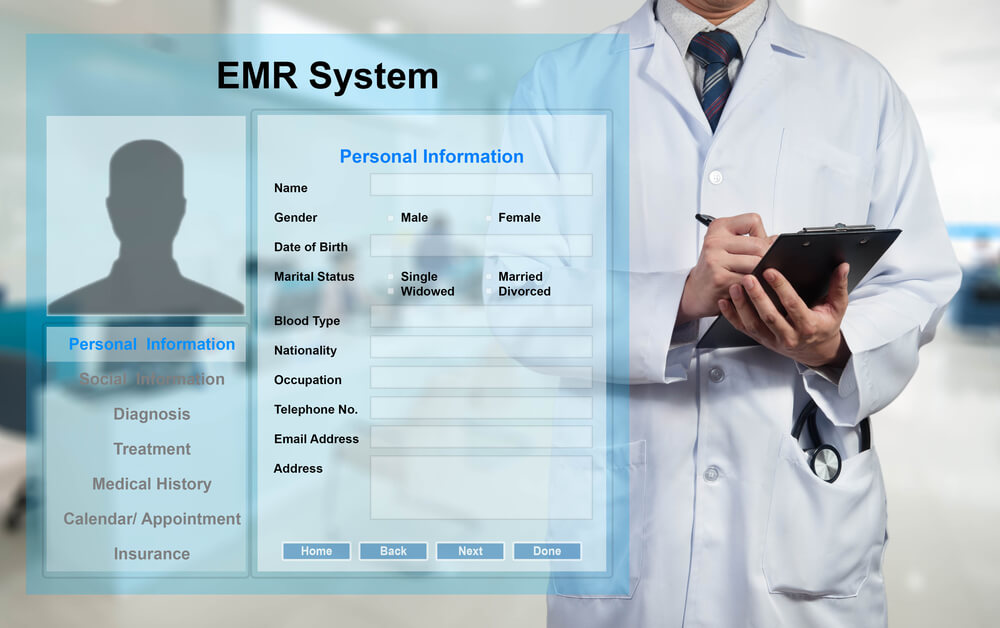
An Electronic Medical Record (EMR) system is a digital version of a patient’s paper chart. It contains the medical and treatment history of patients within a single healthcare practice.
Unlike traditional paper records, EMR systems store comprehensive patient data electronically, making it instantly accessible to authorized healthcare professionals.
Key Components of an EMR System
EMR systems typically include several core features that streamline healthcare delivery:
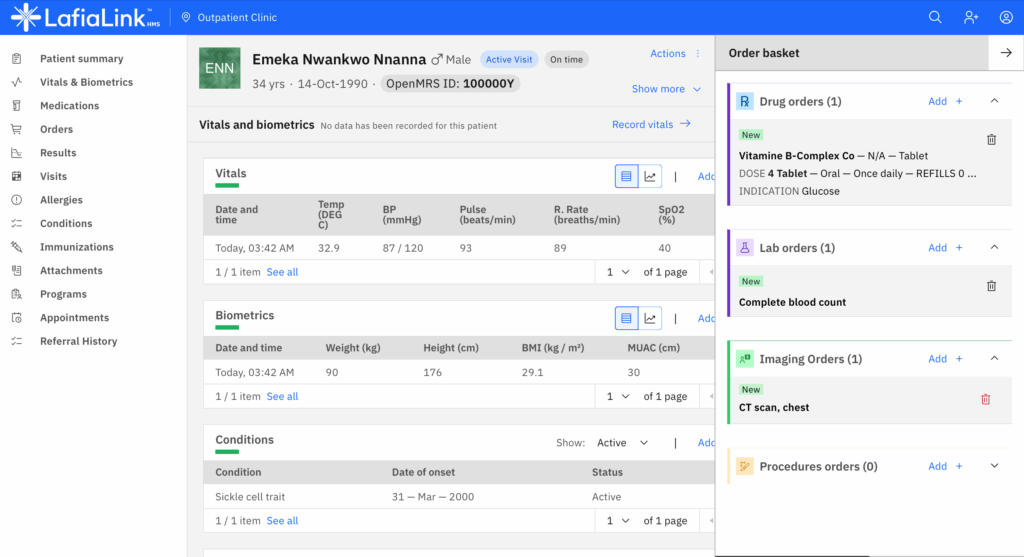
Patient Demographics and History: EMR systems store essential patient information including contact details, insurance information, medical history, allergies, and family health history. This foundational data helps providers make informed treatment decisions.
Clinical Documentation: Healthcare providers can record patient visits, symptoms, diagnoses, and treatment plans directly into the system. This eliminates handwriting interpretation issues and ensures clarity in medical records.
Medication Management: EMR systems track current medications, dosages, and prescription history. Many systems include drug interaction warnings and allergy alerts to prevent medication errors.
Laboratory and Test Results: Lab results, imaging reports, and other diagnostic tests integrate directly into the patient’s record, allowing providers to track health trends over time.
Billing and Coding: Most EMR systems include billing functionality that links clinical documentation to appropriate medical codes for insurance claims and reimbursement.
Benefits of EMR Systems

The adoption of EMR systems brings numerous advantages to healthcare practices and patients alike.
Improved Patient Care: With instant access to complete medical histories, healthcare providers can make better-informed decisions. EMR systems reduce diagnostic errors and ensure continuity of care, especially when multiple providers treat the same patient.
Enhanced Efficiency: Digital records eliminate the time spent searching for paper files. Healthcare staff can access patient information instantly, schedule appointments more efficiently, and process paperwork faster.
Better Coordination: When specialists, primary care physicians, and other healthcare providers use compatible EMR systems, they can share patient information seamlessly, leading to more coordinated care.
Reduced Medical Errors: EMR systems include built-in checks for drug interactions, allergy alerts, and clinical decision support tools that help prevent medical mistakes.
Cost Savings: While initial implementation requires investment, EMR systems reduce long-term costs by eliminating paper, storage space, and administrative overhead. They also improve billing accuracy and reduce claim denials.
Data Security: Modern EMR systems use encryption and access controls to protect sensitive patient information, often providing better security than paper records vulnerable to loss or unauthorized access.
EMR vs EHR: Understanding the Difference
Many people use EMR and EHR (Electronic Health Record) interchangeably, but there’s an important distinction.
EMR systems are digital records used within a single healthcare organization or practice. They contain the standard medical and clinical data collected in that practice.
EHR systems, on the other hand, are designed to share information across multiple healthcare organizations.
EHRs provide a more comprehensive view of a patient’s health and can follow patients to specialists, hospitals, and other care settings.
Common Features in Modern EMR Systems
Today’s EMR platforms offer sophisticated functionality beyond basic record-keeping:
E-Prescribing: Providers can send prescriptions electronically to pharmacies, reducing errors from illegible handwriting and improving medication adherence tracking.
Patient Portals: Many EMR systems include patient-facing portals where individuals can view their records, schedule appointments, communicate with providers, and access test results.
Clinical Decision Support: Advanced EMR systems provide evidence-based treatment recommendations, preventive care reminders, and diagnostic assistance tools.
Reporting and Analytics: Healthcare organizations can generate reports on quality metrics, population health trends, and practice performance to improve care delivery.
Mobile Access: Cloud-based EMR systems allow providers to access patient information from tablets and smartphones, supporting telehealth and care delivery outside traditional office settings.
Choosing the Right EMR System
Healthcare practices considering an EMR system should evaluate several factors:
Practice Size and Specialty: Different EMR systems cater to various practice sizes and specialties. A pediatric practice needs different features than an orthopedic clinic.
Interoperability: The ability to exchange data with hospitals, labs, pharmacies, and other healthcare providers is crucial for comprehensive patient care.
Usability: The system should be intuitive and require minimal training. A complex interface can slow down clinical workflows and frustrate staff.
Compliance: EMR systems must comply with healthcare regulations including HIPAA privacy rules and meet meaningful use requirements for government incentives.
Support and Training: Reliable vendor support and comprehensive training programs ensure smooth implementation and ongoing operation.
Cost Structure: Consider both upfront costs and ongoing expenses including licensing, maintenance, updates, and support fees.
Implementation Challenges
Transitioning to an EMR system presents certain challenges that practices should anticipate:
Initial Costs: Implementation requires significant investment in software, hardware, training, and potential workflow disruptions during the transition period.
Learning Curve: Staff need time to become proficient with new systems, which may temporarily slow productivity.
Data Migration: Converting paper records or transferring data from old systems requires careful planning to ensure accuracy and completeness.
Workflow Changes: EMR systems often require practices to redesign clinical workflows, which can meet resistance from staff accustomed to traditional methods.
The Future of EMR Systems
EMR technology continues to evolve with emerging healthcare trends. Artificial intelligence and machine learning are being integrated to provide predictive analytics, automate documentation, and identify health risks earlier.
Voice recognition and natural language processing are making data entry faster and more natural for clinicians.
Interoperability standards are improving, making it easier for different EMR systems to communicate.
This creates a more connected healthcare ecosystem where patient information flows seamlessly across care settings.
Telehealth integration has become increasingly important, with EMR systems incorporating video consultation capabilities and remote monitoring data directly into patient records.